Editor’s note: This story has been updated to reflect current COVID-19 vaccine eligibility in Indiana.
COVID-19 vaccine distribution is underway in Indiana, and people understandably have a lot of questions.
In December, two COVID-19 vaccines – one developed by Pfizer and one by Moderna – were authorized by the U.S. Food and Drug Administration for emergency use.
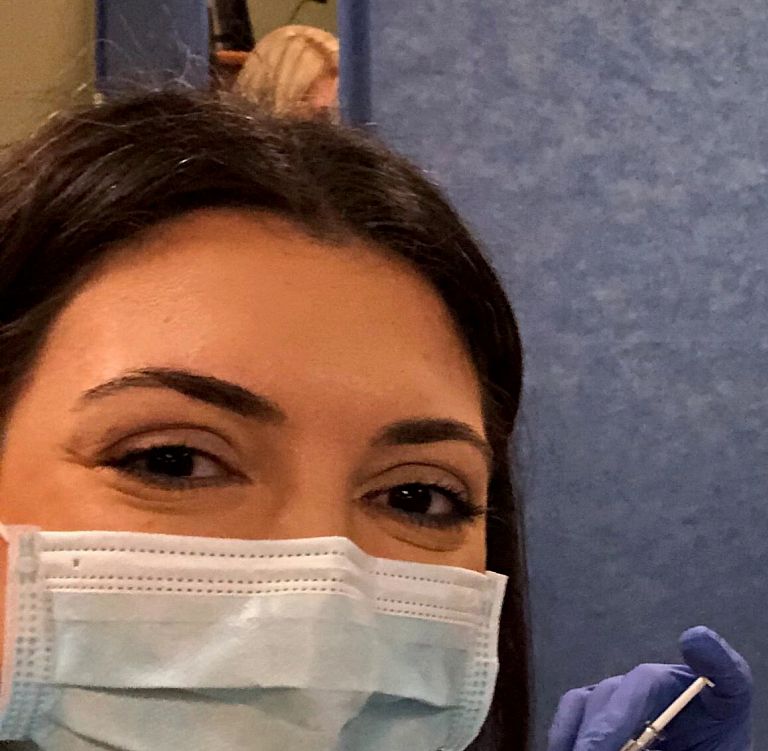
This has been exciting news for many, providing a promising path forward. It’s especially exciting as we approach nearly a year of following public health guidelines to protect ourselves and our communities from COVID-19, and as the number of positive cases and related deaths in our state continues to climb.
It can be difficult to keep up with all of the information – and misinformation – available, so we talked to Dr. Lana Dbeibo, director of vaccine initiatives for Indiana University’s COVID-19 Medical Response Team and an assistant professor of infectious diseases in the IU School of Medicine, to set the record straight. She answers common questions about COVID-19 vaccines, as well as how their arrival is expected to affect life at IU.
Question: Are the COVID-19 vaccines safe and effective?
Answer: According to the FDA and the U.S. Centers for Disease Control and Prevention, data from the manufacturers and large clinical trials have shown no major safety concerns for people who’ve received the Pfizer or Moderna vaccines.
The COVID-19 vaccines are messenger RNA vaccines, or mRNA vaccines, which researchers have been studying for more than a decade to try to prevent other infectious diseases such as flu, Zika and rabies. In the case of COVID-19, these vaccines put an inactive piece of the virus into your body with instructions for your cells on how to create a harmless piece of the coronavirus. Your body’s immune system notices this harmless piece is not supposed to be there and begins to develop antibodies against it, which help your immune system remember how to fight off the real coronavirus should you become infected.
Both manufacturers report their vaccines show approximately 95 percent efficacy at preventing both mild and severe symptoms of COVID-19.
You must receive two doses of the COVID-19 vaccines – either 21 or 28 days apart, depending on which vaccine you get – for the vaccine to be effective. Protection begins seven to 14 days after receiving your second vaccine dose.
Q: How were the vaccines developed so quickly?
A: There are several reasons the COVID-19 vaccines were able to be developed rapidly, many of which have to do with the extraordinary circumstances of everyone working together to try to stop a pandemic. At the same time, it’s important to note that none of these reasons included any bypassing or relaxing of the normal scientific process for vaccine development.
The vaccines were still tested per the normal phases of scientifically rigorous clinical trials, for which they were studied among large and diverse populations, before being made available to the public. These clinical trials were completed much faster than is typical because the pandemic made people more interested in and aware of opportunities to volunteer for the vaccine studies. Scientists often wait many months and sometimes even years to get people to volunteer to be part of clinical trials.
The global prevalence of COVID-19 cases also meant there was a high level of disease – millions of people in the U.S. alone – in the community, which made it much easier for scientists to test the effectiveness of the vaccines faster.
Production of the vaccines was expedited as well. One of the benefits of mRNA vaccine technology is shorter manufacturing times because, unlike many traditional vaccines, they do not use an infectious element and can be developed in a laboratory using a DNA template and readily available materials – a process that can be scaled up more quickly than traditional vaccines.
Production of the vaccines also started earlier in the process than is typical. Usually, manufacturers wait to start production until after the phase 3 clinical trials are completed, just in case. However, because of the urgency of the pandemic, Pfizer and Moderna started producing their vaccines earlier, which is why we had supplies of vaccine ready soon after they were reviewed and authorized by the FDA.
Q: What are the side effects? Can the vaccines give me COVID-19?
A: No, the vaccines cannot give you COVID-19 because they don’t contain any of the live virus (SARS-CoV-2) that causes the disease.
They also do not interact with or affect your DNA in any way; mRNA from the vaccine never enters the nucleus of your cells, which is where your DNA is stored.
Side effects that you might experience are mild and include soreness at the injection site, fever, fatigue, muscle pains, joint pains or headaches. If you develop side effects, they would appear 24 to 48 hours after you receive a vaccine dose and can last up to 24 hours. People typically experience a greater immune response after the second vaccine dose.
If you start to develop these symptoms more than 48 hours after receiving the vaccine, or if they last for more than 24 hours, then this could be unrelated to the vaccine; it’s recommended that you stay home and contact your doctor or the IU Health Virtual Screening Clinic.
The CDC is interested in knowing more about any side effects people experience after getting a COVID-19 vaccine. If you’ve been vaccinated, you can help the CDC by participating in daily health check-ins on your smartphone.
Q: Is there anyone who shouldn’t get a COVID-19 vaccine? What about people with allergies or those who are immunocompromised?
A: The Pfizer vaccine is currently not authorized for children under age 16, and the Moderna vaccine is not authorized for those under age 18.
According to the CDC, anyone who has a history of a severe allergic reaction, also called anaphylaxis, or immediate allergic reaction to any of the mRNA vaccine ingredients should not receive these vaccines.
Other than a history of anaphylaxis to mRNA vaccines or components of these vaccines, allergies are not listed by the CDC as a contraindication to getting a COVID-19 vaccine. The CDC considers a history of any immediate allergic reaction to any other vaccine or injectable therapy as a precaution but not a contraindication to vaccination. Everyone who receives either one of these vaccines will be monitored for 15 to 30 minutes in the clinic, because serious allergic reactions will happen in the first few minutes after the vaccine is given.
While the efficacy of the COVID-19 vaccines was not studied in immunocompromised people, the danger associated with actually getting COVID-19 is very high for people with weaker immune systems. Because the benefit may exceed the risk, the CDC did not list being immunocompromised as a contraindication to receiving a COVID-19 vaccine.
If you have questions about your individual medical history, please consult with your physician to have a conversation about this.
Remember that scientific observations of the vaccines are ongoing. The CDC, FDA and other government agencies will update the public about significant changes, if they occur.
Q: When can I get a vaccine? Can IU decide who is eligible?
A: As of March 31, 2021, everyone in Indiana 16 years old and above is eligible to receive the vaccine.
Eligibility is determined by the state of Indiana, and IU cannot make exceptions for any of our faculty, staff or students.
Q: Is IU administering any COVID-19 vaccines?
A: Yes, Simon Skjodt Assembly Hall on the IU Bloomington campus is now a vaccine site both open to the community as well as IU Bloomington students, faculty and staff. IUPUI will soon be offering vaccine appointments for IUPUI students, faculty and staff. Several of IU’s regional campuses are working with their local health departments and other partners to ensure vaccine appointments are available on or near campus.
Q: After I’m vaccinated, can I stop following public health guidelines? Do I still have to participate in IU mitigation testing and contact tracing?
A: Clinical trials have shown that the vaccines reduce your risk of developing illness due to COVID-19. However, being vaccinated does not provide perfect protection. Additionally, we don’t yet know how long protection from the vaccine lasts or whether people who are vaccinated can still be asymptomatically infected (no symptoms) and therefore spread the virus to others.
Because of all of these reasons, even if you are vaccinated, you will still need to continue safe behaviors such as wearing face masks, staying at least 6 feet apart from others and washing your hands frequently to help stop the spread of COVID-19. As a member of the IU community, you will also still be required to participate in the university’s mitigation testing and contact tracing efforts to help keep our campuses safe.
This guidance will continue until we have more scientific information about the duration of immunity and until the majority of the population is vaccinated, which is what it would take to achieve herd immunity.
For more information, visit the FAQ page on the covid.iu.edu site.

